Dr Juliana Maynard is Head of Translational Imaging at Medicines Discovery Catapult (MDC) and Director of Operations and Engagement for the National PET Imaging Platform.
This is the first in a series of radiopharmaceutical blogs from Dr Juliana Maynard. Juliana is an expert imaging scientist with over 20 years’ experience in nuclear medicine and translational imaging.
January 2026

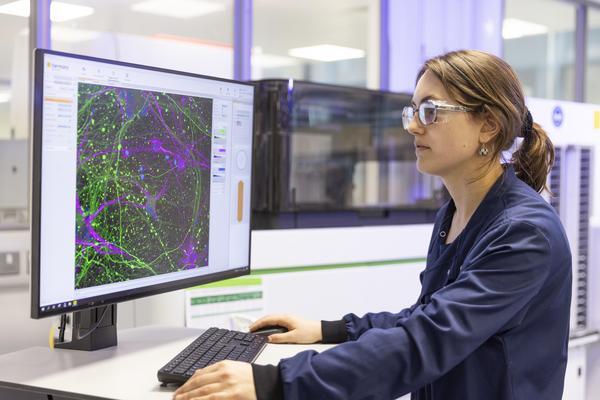
Throughout my career, my radiopharmaceutical work has spanned all stages of development, from target biology, distribution, and dosimetry to translational modelling and clinical use. Despite this varied experience, I have mostly been driven by one objective: ensuring that preclinical data do more than simply demonstrate scientific promise. A core part of my role here at MDC is helping innovators design studies that answer the questions that they, investors and regulators care about most, early enough to enable decision-making, drive clear outcomes, and reduce risk in radiopharmaceutical development. We do this using our broad and deep experience of working alongside industrial clients with our end-to-end platform that incorporates radiochemistry, cutting-edge imaging capabilities and data interpretation.
Radiopharmaceuticals sit at the intersection of biology, physics, and medicine. This unique convergence creates a level of complexity that can make it difficult for some investors to distinguish genuine value from early-stage promise. In this field, early data can vary widely in value. Some datasets are simply descriptive, but others go much further, providing real confidence in decision-making around the asset and helping to de-risk investment.
The difference matters.
For radiopharmaceutical programmes, the most investable preclinical packages are not necessarily those with the strongest signal in a single study, but those that answer five fundamental questions:
In practice, many programmes attempt to answer these questions, but fall short due to suboptimal timepoints, underpowered study design, use of isotopes poorly matched to the underlying biology, or a failure to integrate biodistribution, efficacy, and dosimetry data into a coherent translational narrative.
To understand why proper answers to these questions are important to investors, let’s examine each in more detail.
Firstly, investors need clarity on radiopharmaceutical biodistribution. Radiopharmaceuticals are systemic by design, and because they deliver toxic radiation, the question is not simply “does the candidate reach the tumour?” but also “where else in the body does it accumulate along the way?”
High-quality biodistribution data should:
Programmes that can clearly show where a radiopharmaceutical goes in the body, and why, can greatly reduce uncertainty around safety, manufacturability, and clinical feasibility, helping to make sure the right candidates progress into patients.
Even low levels of radiation hitting the wrong tissues can provide an important signal and narrow the therapeutic window long before dose-limiting toxicity is formally observed in clinical studies.
Preclinical data that genuinely de-risk investment go beyond histology snapshots. They integrate:
This level of insight allows investors to assess whether observed risks are intrinsic to the mechanism, or manageable through dose, schedule, or isotope selection.
Data on tumour response alone are insufficient. Investors want to understand not just that the radiopharmaceutical works, but why it works.
Strong preclinical efficacy packages demonstrate:
This mechanistic linkage is critical. It enables rational translation into humans and reduces the probability that early clinical signals are artefactual or non-reproducible.
Unlike most conventional therapeutics, radiopharmaceuticals allow for precise dosimetry modelling, and regulators expect programmes to use this advantage.
Regulators, including the FDA and EMA, have been clear in their radiopharmaceutical development guidance that understanding absorbed dose to both target and non-target tissues is central to safety assessment, first-in-human dose selection, and clinical trial design. Preclinical dosimetry studies that de-risk investment convert biodistribution data into organ-level absorbed dose estimates, support human dose extrapolation, and identify dose-limiting tissues before first-in-human studies.
This approach transforms radiation exposure from an abstract concern into a measurable, optimisable variable, improving regulatory confidence and capital efficiency.
Perhaps the most underappreciated value driver is understanding the minimal effective dose relevant to the targeted outcome, which is the lowest amount of radioactivity that produces a meaningful therapeutic effect in a tumour without causing harm to healthy tissues.
Programmes that can demonstrate a meaningful biological effect at lower doses can unlock:
Preclinical dose-response data that identify the lowest biologically active dose provide this strategic optionality, and optionality is what ultimately drives premium radiopharmaceutical valuations.
Preclinical data generation should not be viewed as just a scientific hurdle. It is also one of the most powerful instruments for managing risk and attracting investment in radiopharmaceutical development. Biodistribution, off-target exposure, mechanistic efficacy, dosimetry, and minimal effective dose together form the backbone of a credible radiopharmaceutical investment thesis. Teams that get this right don’t just progress their asset; they accelerate value creation and reduce the capital required to reach clinical validation.
If you would like more information or would like to discuss your study design and execution using our integrated radiopharmaceutical evaluation and characterisation platform, please get in touch and see how MDC can make your next move count.
Our experts are here to support your radiopharmaceutical journey from concept to clinic.
Speak to us to see how we can help advance your drug discovery project.
Find out more about how we can help
In this blog, Dr Phil Auckland details how MDC has established a reproducible CRISPR-Cas9 pipeline and generated new tools to better inform nanotherapeutic design
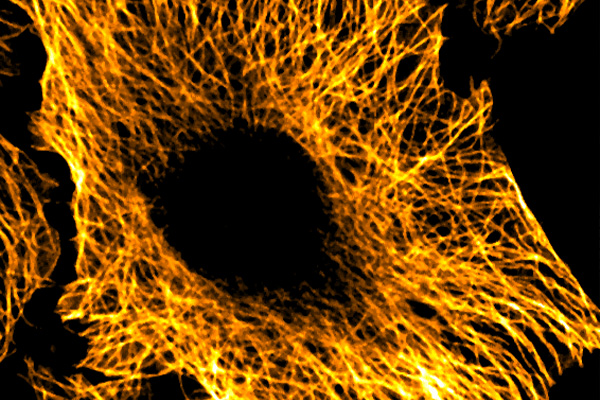
Nanotherapeutics often fail because of Endosomal entrapment. In this blog by Dr Phil Auckland, we explore how MDC are using real-time imaging to reveal why.
Accelerating analgesic development through human-specific in vitro systems