Rare diseases in the European Union
Increased awareness of rare diseases and a favourable investment environment for orphan drug development represent opportunities for academic research and SMEs. To convert this potential into patient benefits, research impact and financial revenue it is essential to understand this topic in-depth and navigate pivotal regulatory processes, such as the Orphan Drug Designation.
The general perception of orphan diseases is that they affect an extremely small number of people and that there is very little that can be done to help those who are predisposed to such a condition. Most people consider an orphan disease to be something that happens to someone else, is severe and has no cure or even rudimentary treatment options.
This over-simplification of orphan diseases is completely misleading. It’s no exaggeration to view orphan diseases as a global health issue when their combined impact is examined. Orphan diseases can present at any age and can be both acute or chronic. Their aetiology is not just genetic, but could be the result of an immunogenic response, reaction to a toxin, an adverse drug reaction or a consequence of an infection.
“Approximately 250 million people globally suffer from an orphan disease; within the EU, 30 million people suffer from a rare disease.”
It is important to remember the range of people and causes of orphan diseases, the majority have an established genetic link (80%) and 50% effect children. The prevalence of each condition ranges from single figures to 24,500 in the EU. At the upper end of this scale this is approximately the equivalent of a city with the population of Strasbourg suffering from a rare disease.
Why is orphan drug development important?
The importance of orphan drug development is magnified by the severity typical of these diseases and the unmet clinical need, leaving these patients without any treatment options. Physicians frequently discuss the bittersweet of being able to provide an accurate diagnosis for a patient after sometimes years of uncertainty, which instead of helping them only emphasises the futility of their situation.
There are an estimated 5000-8000 rare diseases globally for which an orphan drug can currently be developed. Whilst rare diseases will not yield the financial returns of blockbuster drugs, the evolution of targeted therapies in the mainstream pharmaceutical industry allows development of investigational treatments for conditions of low prevalence to be a more acceptable business opportunity to investors. Patients with a rare disease and their families are often tireless campaigners for their advancement of treatment options and research is strongly supported by public and charitable funding.
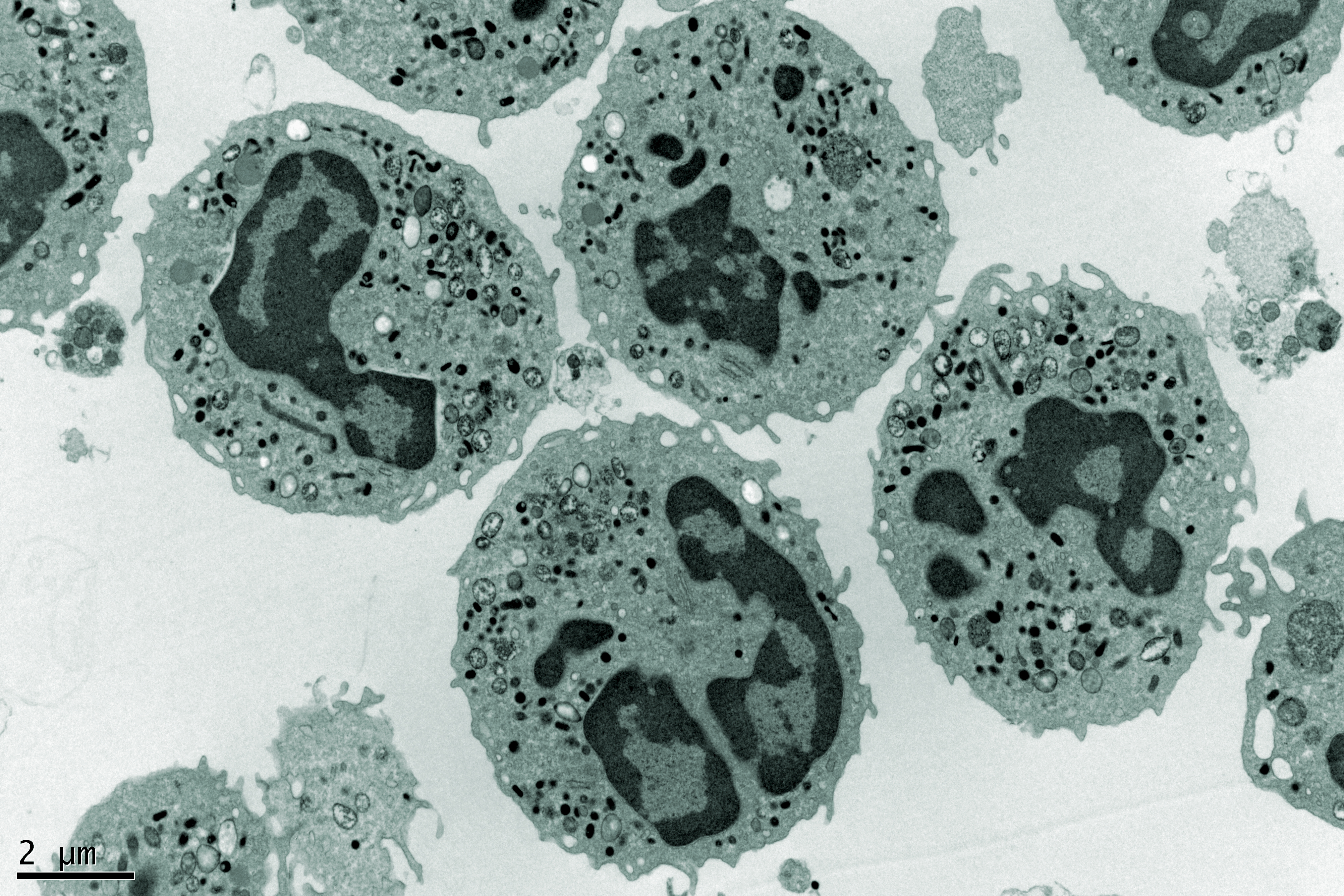
The emergence of advanced medicines using cells, tissue or gene therapies has also acclimatised ‘payers’ to the hefty costs of transformative drugs. These would typically have been well outside of the approved cost structures of public healthcare providers.
“Patients are often young with associated non-drug treatment costs that can be exceptionally high.”
With 80% of orphan drugs having a genetic link, the advancement and refinement of gene therapies provides a potential new source of treatments for these orphan diseases. Furthermore, given the desire for regulators to accelerate the translation of scientific breakthroughs into patient benefits, orphan diseases present an opportunity for industry to refine and validate advanced cell and gene therapies whilst providing treatment options where none exist.
The main commercial incentive is a flexible and favourable regulatory framework to support the manufacture, testing and commercialisation of orphan drugs. These flexibilities are in place to support the rights of these patients to adequate healthcare provision and any loosening of regulatory control is proportionate to the risks and benefits of the proposed intervention and the alternative options.
Orphan drug designation
Orphan drug development refers to the process through which therapeutic agents are discovered, tested and marketed for clinical indications that would not be ‘economically’ viable to produce.
There is a regulatory process for the classification of these drugs that is formally known as the ‘Orphan Drug Designation’ in the EU. It is this designation that allows developers to access dedicated funding streams and benefit from the regulatory and commercial advantages afforded to orphan drug development within the EU.
Orphan drug classification varies between regions although there are fundamental similarities. In the EU to obtain orphan drug status, Articles 3&5 of the Orphan Drug Regulation must be met. The following criteria is applied:
- The product is for a life-threatening or chronically debilitating condition with a prevalence no greater than 5 in 10,000 within the European Community
- If no incentives are granted the return on development costs are likely to be insufficient
- There is no satisfactory alternative or the applicant’s product should represent a significant benefit
In the EU orphan drug designation is through a centralised process. An application is made to the EMA using a standardised dossier format available through their website. A multidisciplinary group called the Committee for Orphan Medicinal Products (COMP) are responsible for reviewing all orphan drug applications. The Group is composed of 1 member from each Member State, 3 members from the EMA, 1 member from both Iceland and Norway. Additionally, the group are supported by experts and patient representatives. The procedure is free of charge and detailed below:
- Sponsor contacts the EMA at least 2 months prior to the submission date
- Sponsor and EMA engage through pre-submission meeting
- Sponsor submits application by submission deadline date
- EMA validate the application (30 days) and ‘start the clock’ on the review (day 0)
- The application is assigned to 2 reviewers for review – 1 from the EMA and 1 from the COMP
- Prior to day 60 a draft summary is distributed to the other members of COMP
- On day 60 the application is discussed with a positive decision given or further information requested
- On day 90 the application is discussed again, and the Sponsor is offered the chance to comment on the application and any further information that was requested.
- A decision is then made with four outcomes possible:
- Approval
- Rejection
- Rejection that is appealed
- Rejection with resubmission
- The European Commission adopts the opinion within 30 Days
An approved orphan drug designation can determine the feasibility of continued development. Some of the essential elements that will be reviewed in greater detail in Part 2.
About the author
Stephen Liggett is the Regulatory Services Manager for Venn Life Sciences.
He is driven to translate scientific innovation into healthcare products, delivering patients benefits. Previously, he acted as a consultant to a wide variety of innovative companies operating in the Pharma, Biotech and Medical Device Industries. Stephen worked in the NHS, industry and academia having taught Regulatory Affairs internationally.
He has been recognised by industry through the TOPRA Futures award in 2016 for his work on cell therapies and other cutting-edge regulatory projects. The MHRA also have a case study featuring his involvement in developing a Microneedle Array Patch and he has several publications on translating research into healthcare products.
In his role at Venn Life Sciences, Stephen uses his regulatory and technology transfer expertise to support research groups in academia and industry. Stephen holds an MPharm and PhD from Queens University Belfast.