Just a few years ago the idea of stem cells was seen more as science fiction than science fact. The general public as a whole didn’t really know what stem cells were, or why they were being used. Even today, when speaking to people outside of the life sciences area about my work, they often give me a disapproving look initially and talk about embryos and growing ears on mice (the common misconception that still lingers on!). However, when I explain how far the field of stem cell research has advanced over the last 10 years, and what we are able to achieve today, they get excited, and quite rightly so!
Life scientists working in a broad range of research areas are now using stem cells to answer biological questions that were previously unknown. So much so that stem cell biology has quickly become the new ‘trendy’ science. So how did this change come about?
Just over 10 years ago in 2007, two labs independently identified a method to make human stem cells without the use of human embryos. This was a huge leap in the field, allowing what are now called induced pluripotent stem cells (iPSCs) to be made from any adult somatic cell type. These iPSCs are equivalent to the previously used embryonic stem cells and can be instructed to become almost any cell type in the human body.
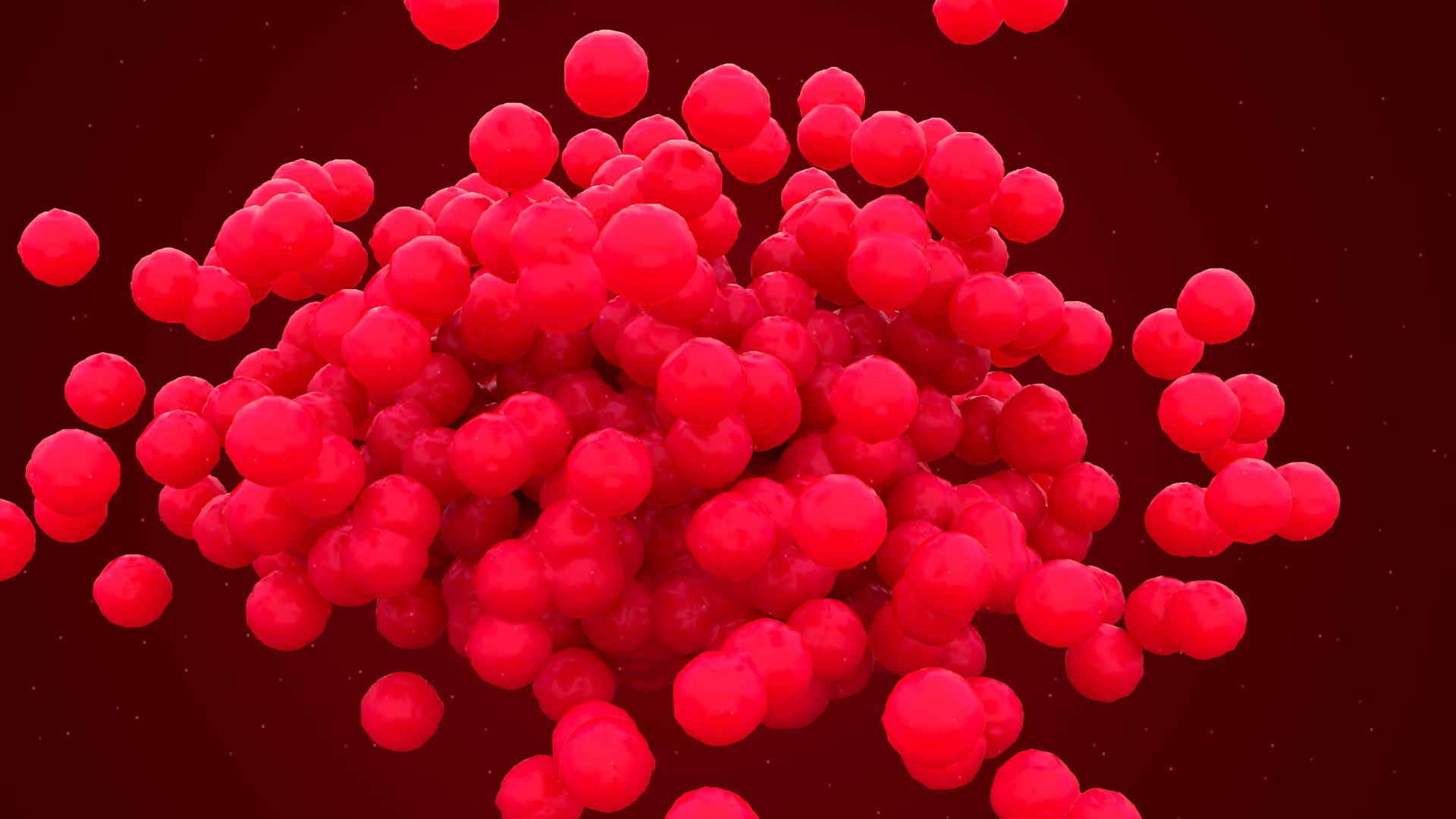
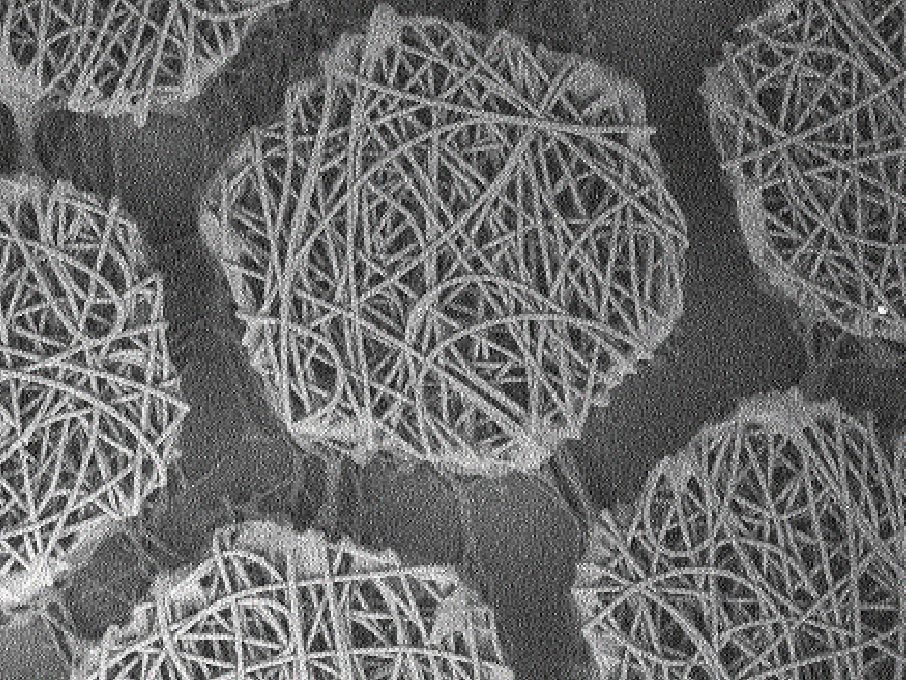
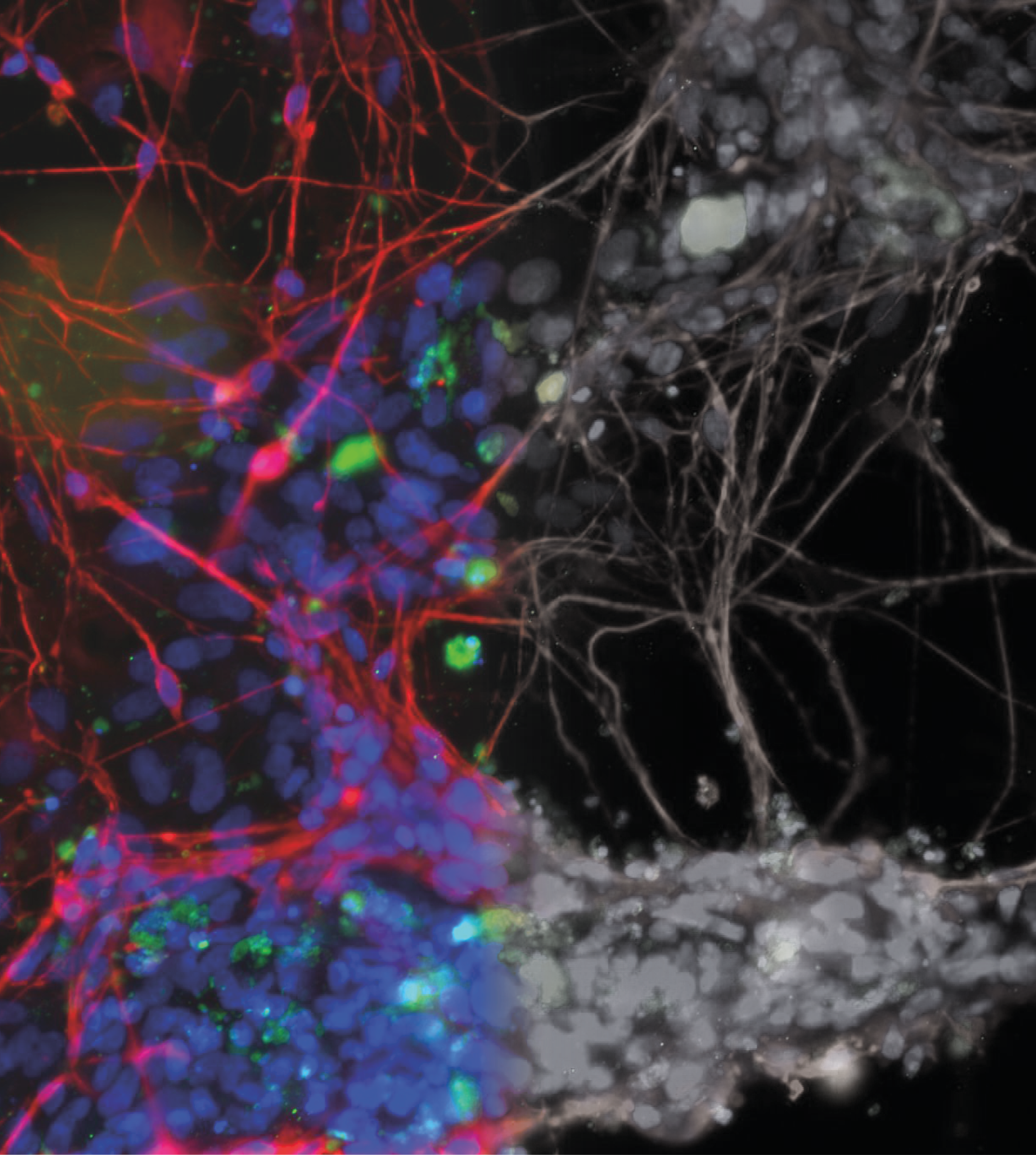
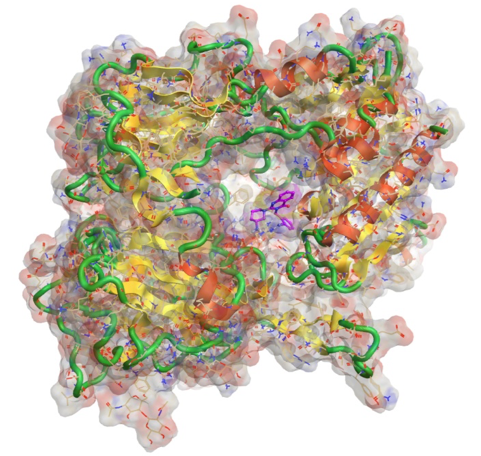
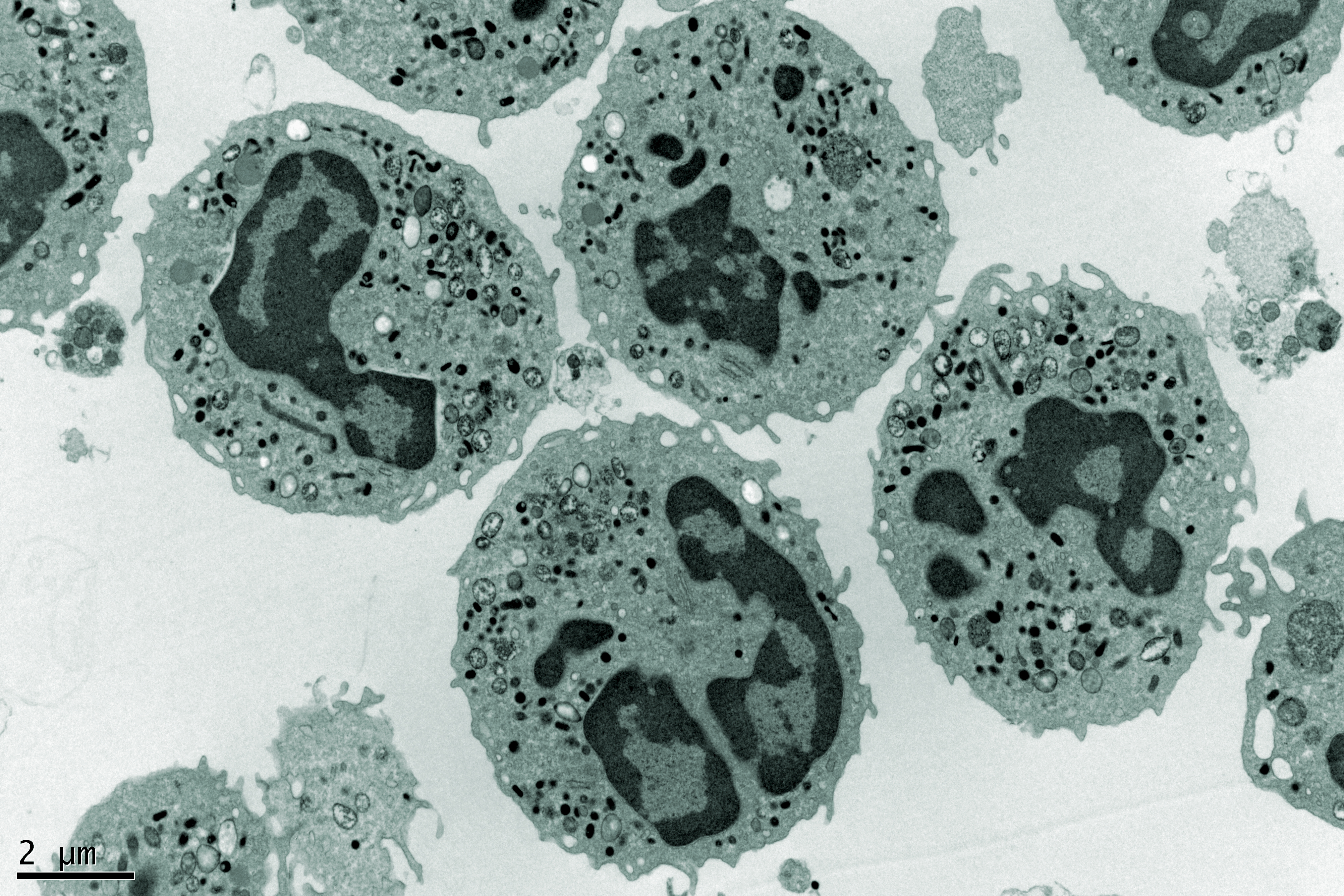
This is achieved by growing iPSCs in the lab and mimicking the instructions those cells would have received in the human body during development, a process called differentiation. The directed differentiation of stem cells has been a major area of interest in the stem cell field, and as a result there are now robust methods to make a wide range of cell types from stem cells. Not only can single cell types be derived from iPSC, but multicellular 3D structures can also be made, known as organoids.
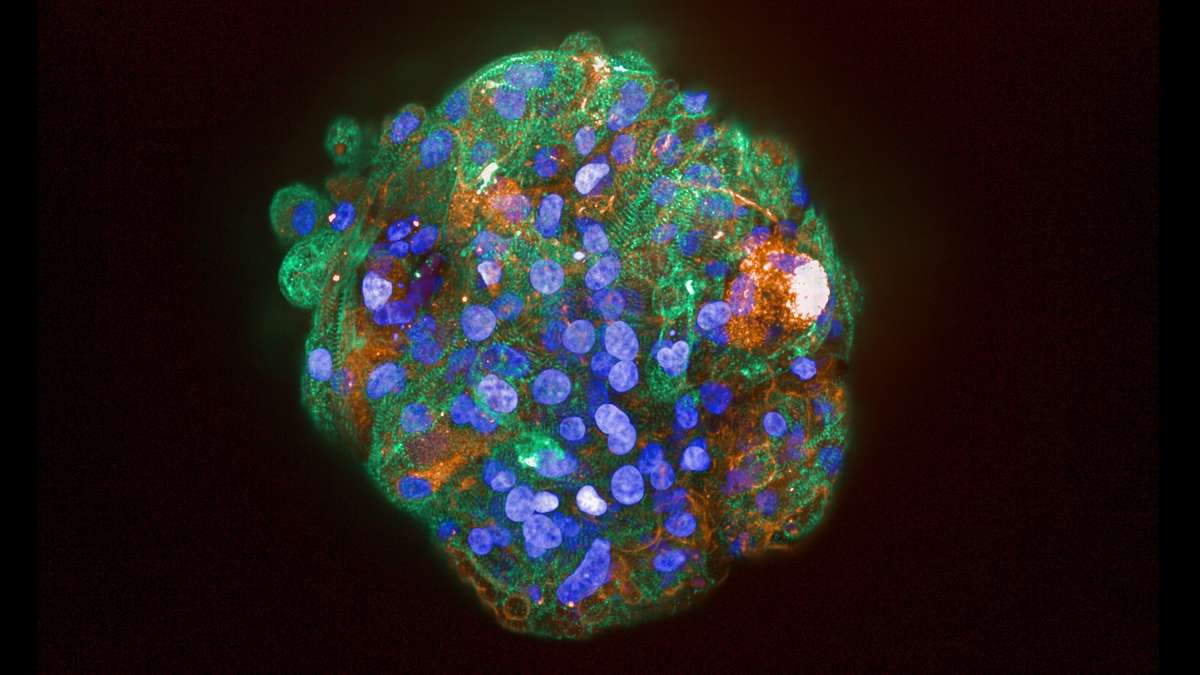
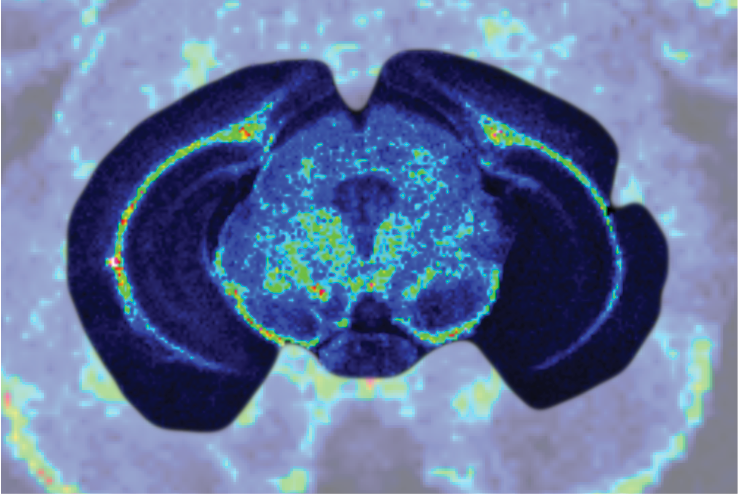
Organoids are formed from differentiated iPSCs and represent accurate small-scale models of developing human organs, including the eye, brain, intestine, stomach, liver, lung, kidney and heart. These ‘mini-organs’ have allowed scientists to study human development in previously unimagined detail and are now being taken a step further to study the mechanisms of human disease in a dish.
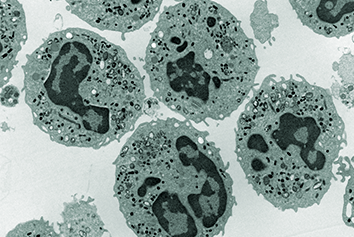
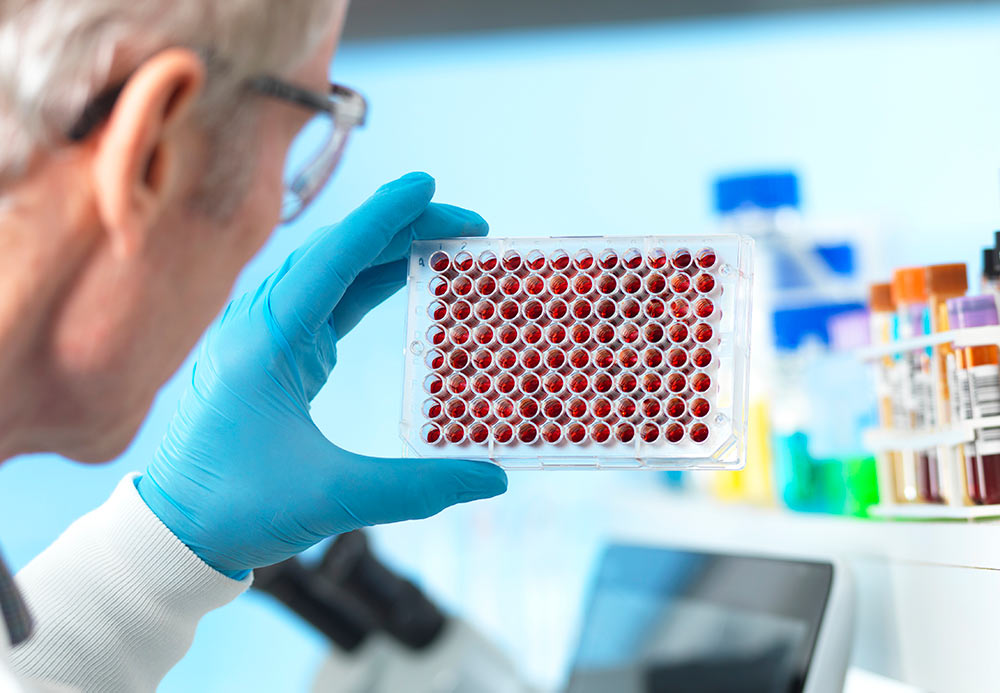
iPSC can be made from a simple skin or blood sample so can be created from any individual. They also have the added benefit of retaining the genome of that particular person, and as such are able to model certain genetic diseases in a dish. A number of laboratories have now successfully used such organoids to investigate how diseases progress, and how we can potentially intervene in these disease processes in order to develop new therapeutics.
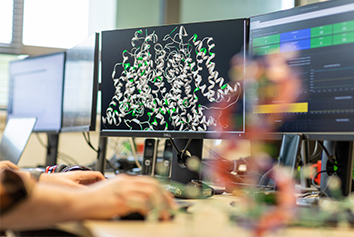
Historically, drug discovery has been performed in ‘simple’ flat layers of cells and in animals. Whilst there have been many successful drugs developed using these models, over the years the attrition rate has soared to the point that failure is almost expected, and success is a rarity. This directly reflects the models which are being used to identify new drug targets and successful molecules, as both cells grown on a layer of plastic and animal models often do not accurately replicate what happens in a human patient.
The advent of iPSC technology now provides an avenue through which human 3D cell models can be implemented in the drug discovery pipeline. These human iPSC-derived organoids closely recapitulate the human condition and will provide a more informative cell model to be used in the early stages of drug development.
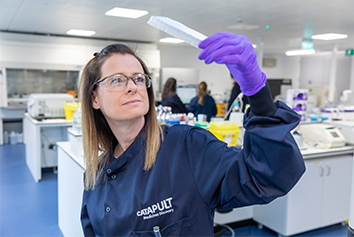
At Medicines Discovery Catapult we are building a suite of complex human cell models to address this need, which we will provide to UK SMEs to accelerate their drug discovery research with the aim of developing better medicines, faster.
About the author
Dr Lorna Hale is Lead Scientist in Stem Cells & Complex Biology at Medicines Discovery Catapult.
She has worked in the field of Renal medicine for over 10 years, with a focus on the role of the glomerular podocyte in kidney disease. Her research has utilised a wide range of in vitro and in vivo models, more recently focusing on induced pluripotent stem cell (iPSC)-derived organoids.