In the previous article, we established the procedural aspects of EU Orphan Drug Designation. Now let’s look at what elements of orphan disease applications require a more detailed review by COMP (Committee for Orphan Medicinal Products).
Prevalence of the disease
This definition is quite clear, but it’s important to understand how the terms of classification criteria influence the ongoing development of a drug. In relation to prevalence, it’s mandatory within the EU to base this on the whole community, and not just to use data from a couple of countries. Prevalence is not something that can be ‘fudged’ and is reviewed in collaboration with expert advice that draws on current evidence.
It’s important to realise that the orphan drug designation is not held indefinitely. Should a disease be classed more prevalent than previously reported the orphan drug designation will be withdrawn.
As understanding of the disease and information about the orphan drug becomes available, clinicians are better informed and more likely to provide a diagnosis for the condition. It’s also possible for the condition to be recognised as a subset of a more prevalent disease that removes the orphan status in the EU. Any calculation of prevalence should reference the EMA guidance.
A medical condition might seem like an obvious term but, within the context of eligibility as an orphan drug, it should be distinct with a specific pathophysiological profile and clinical prognosis. An essential consideration for EU orphan drug designation is not being a subset of a more prevalent condition.
Orphan designation considerations
Essential similarity
The granting of a Marketing Authorisation for a medicinal product with an Orphan Drug Designation gives market exclusivity in Member States for a period of 10 years. During this time no applications will be received for the same therapeutic indication for a similar medicinal product. Similarity is judged by applying the following 3 criteria:
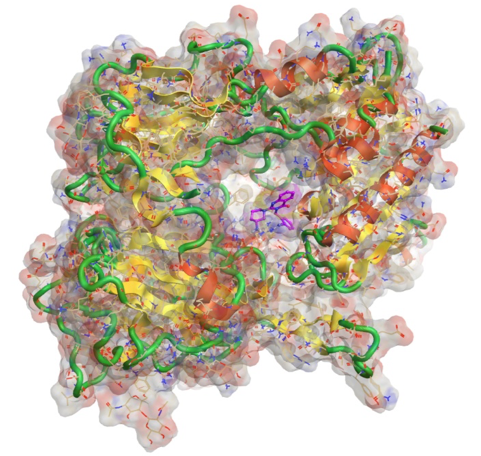
- Molecular structure
- Mechanism of action
- Therapeutic indication
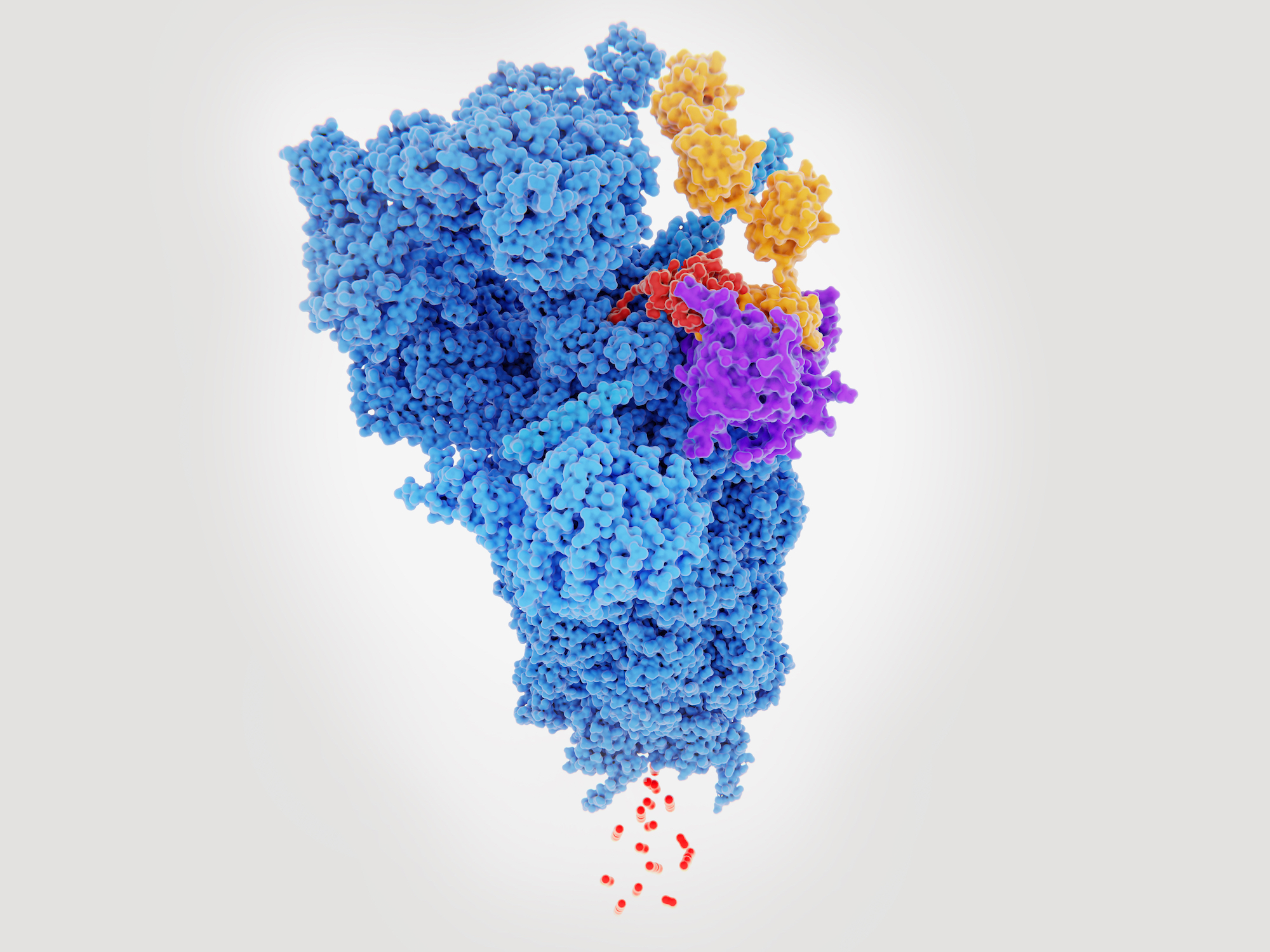
When considering chemical-based actives this is quite a simple determination, but for cutting-edge technologies such as advanced therapies it’s more difficult to separate some actives based on these three criteria.
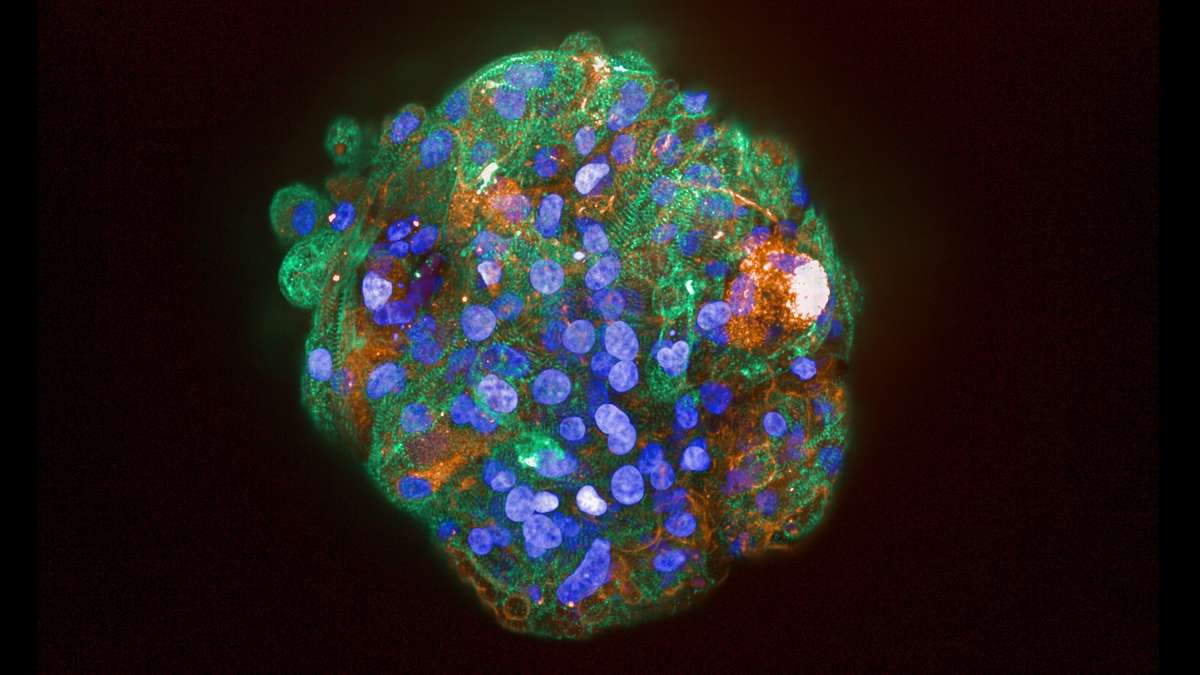
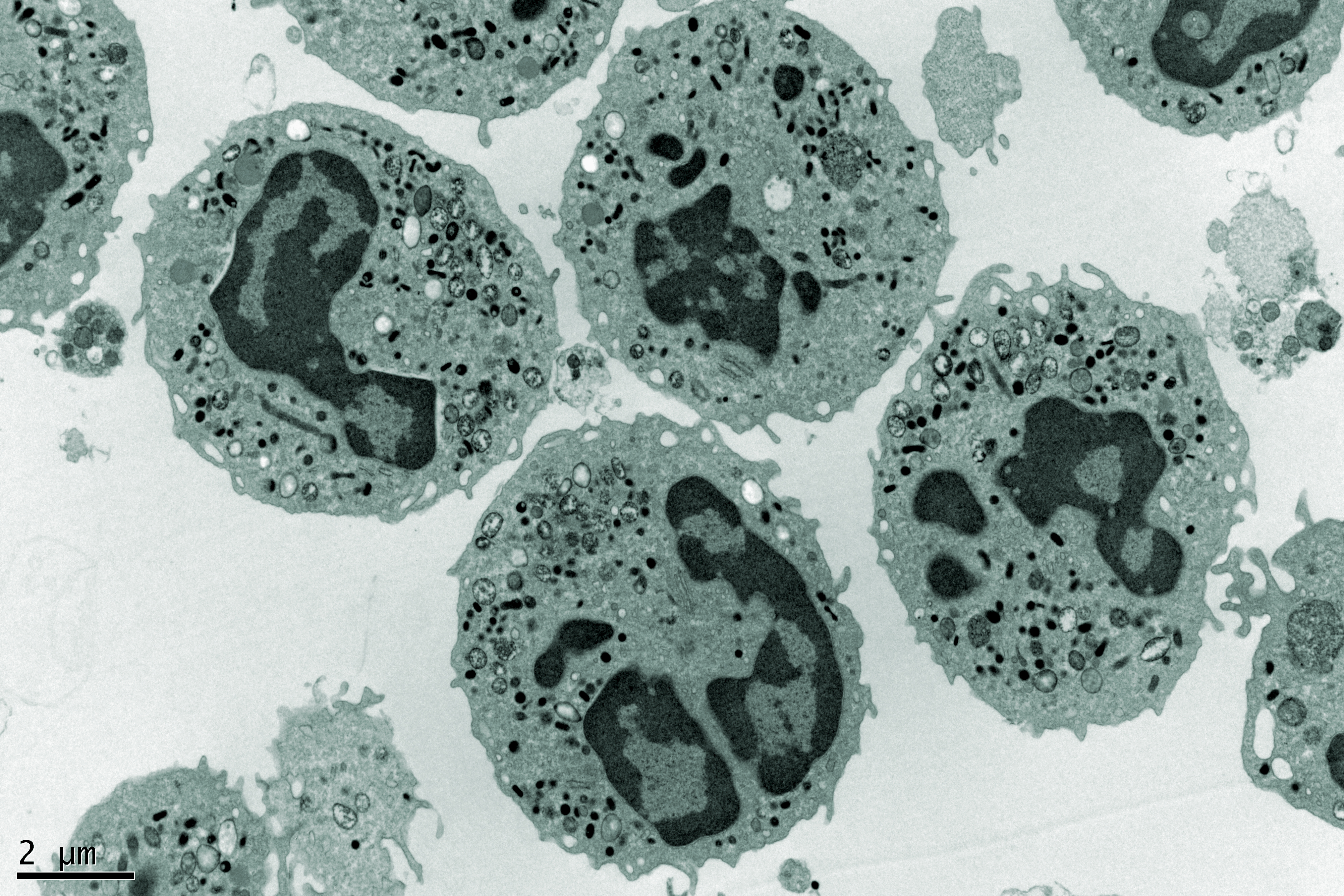
For instance, a cell therapy may be characterised based on a specific trait, to provide a drug product that is distinct from other cells of the same general type e.g. Mesenchymal stem cells (MSC). However, if the trait does not confer any therapeutic advantage and is merely a means to standardise the cell population into a more acceptable pharmaceutical form then the possibility exists for a competitor to generate a MSC product with a different profile.
Whilst the original clinical trials cannot be referenced in a Marketing Application the developer of the new MSC therapy would be at an advantage to the originator product as they would already know the cell therapy is likely to provide a clinical benefit based on the Marketing Application Authorisation and the relevant European Public Assessment Report.
The progress in advanced therapies and the impact on essential similarity related to orphan designation by the EMA is further explored in this EMA Q&A document.
Significant benefit
There must be a robust rationale for using the drug in the rare disease and it must be proven to demonstrate significant benefit over all other therapies at the time of Marketing Authorisation.
The Sponsor of the orphan drug will usually engage with the EMA through protocol assistance to establish what the regulator considers as significant in their specific case. Significant benefit and favourable risk:benefit is entirely different, and these terms must be understood to establish a successful clinical validation of the orphan drug. An approval of a ‘normal’ Marketing Application will depend on the applicant establishing that the clinical benefit to the patient of using the product and the risk of taking it are no worse than the products currently available on the market. For an orphan drug, the review is not as straight-forward because significant benefit must be established.
In other words, the orphan drug must present a significant benefit to the patient and cannot simply provide an equivalent treatment option.
Significant benefit doesn’t just mean improved clinical efficacy but could be improved convenience to the patient. The route of administration may be more convenient, there may be reduced monitoring of patients, reduced side-effects, the product may be significantly cheaper or perhaps the manufacturing method offers significant advantages around accessibility.
Incentives for orphan drug designation
The incentives available to encourage orphan drug development have led to established orphan drug divisions in most medium-large pharmaceutical companies. Fee reductions are based on the financial standing of the sponsor and make it viable for micro, small and medium sized companies to commercialise their orphan drug. The EMA class an organisation with less than 250 staff and a turnover of under 50 million euro as an SME.
Fee reductions include the scientific advice procedure – specifically developed for orphan drugs called protocol assistance – but extend to Marketing Authorisation Applications, annual fees, pre-authorisation inspections and variations. Protocol Assistance optimises the development programme and improves the probability of a Marketing Authorisation being granted.
Regulatory flexibility and fee reductions are not the only carrots dangled in front of drug developers. An extended period of exclusivity of ten years is also offered with a further two years on completion of a Paediatric Investigation Plan. The standard time limit in the EU for a new drug is eight years with 2 further years for a successfully executed PIP.
There is a substantial level of funding available for investigating orphan drugs in programmes such as Horizon 2020 and the European Joint Programme on Rare Diseases.
The Wellcome Trust also have a Pathfinder Award Program. To be eligible for this programme the applicants must hold an ‘Orphan Designation’ from the European Medicines Agency (EMA) and incorporated protocol assistance into their clinical trial programme. Additionally, there are multiple funding opportunities from Venture Capitalists specialising in Orphan Drug Development.
Summary orphan drug designation and drug development
Patients suffering from life-threatening and chronic debilitating diseases deserve the same access to medicines as those with more prevalent conditions. To enable this access regulatory frameworks throughout the world have been developed to reduce barriers to development. Whilst the focus of this review has been the EU, the US and Japan have comparable schemes and submission in parallel is encouraged by the EMA.
About the author
Stephen Liggett is the Regulatory Services Manager for Venn Life Sciences.
He is driven to translate scientific innovation into healthcare products, delivering patients benefits. Previously, he acted as a consultant to a wide variety of innovative companies operating in the Pharma, Biotech and Medical Device Industries. Stephen worked in the NHS, industry and academia having taught Regulatory Affairs internationally.
He has been recognised by industry through the TOPRA Futures award in 2016 for his work on cell therapies and other cutting-edge regulatory projects. The MHRA also have a case study featuring his involvement in developing a Microneedle Array Patch and he has several publications on translating research into healthcare products.
In his role at Venn Life Sciences, Stephen uses his regulatory and technology transfer expertise to support research groups in academia and industry. Stephen holds an MPharm and PhD from Queens University Belfast.